MACULAR DEGENERATION TREATMENT IN LOUISVILLE
Koby Karp Doctors Eye Institute specializes in the treatment of Macular Degeneration. Whether you are experiencing symptoms or getting information for a relative or a friend, we have provided a great deal of information here to answer some of your questions.
MACULAR DEGENERATION
WHAT IS MACULAR DEGENERATION?
Macular degeneration is a progressive eye condition that affects as many as 15 million Americans. The disease occurs most often in people over the age of 55 years old. This form of the disease is traditionally referred to as Age Related Macular Degeneration (ARMD). In macular degeneration, the light-sensing cells of the macula mysteriously malfunction and may over time cease to work.
Macular degeneration is caused by the deterioration of the central portion of the retina, known as the macula, the inside back layer of the eye that records the images we see and sends them, via the optic nerve, from the eye to the brain. It is responsible for focusing central vision in the eye. The disease robs the individual of all but the outermost, peripheral vision, leaving only dim images or black holes at the center of vision, but it rarely results in complete blindness. It destroys the clear, “straight ahead” central vision necessary for reading, driving, identifying faces, watching television, doing fine detailed work, safely navigating stairs and performing other daily tasks. It can also dim contrast sensitivity and color perception. Peripheral vision may not be affected, making it possible to see “out of the corner of your eye”.
TWO MAIN TYPES OF AGE RELATED MACULAR DEGENERATION

It is not uncommon for a patient with the “dry” form to develop the “wet” form later, so it is possible to experience both forms at the same time, in one or both eyes. The onset and progression of either type do not follow any particular pattern. AMD can be difficult to diagnose in its earliest stages. It can sometimes progress so slowly that people do not notice a change in their vision. They may put off seeing an ophthalmologist or eye care professional for several years. In other cases, the deterioration can be very rapid and can seem to happen overnight.
Dry or atrophic MD reduces one’s central vision and can effect color perception. Generally, the damage caused by the “dry” form is not as severe as that of the “wet” form.
While there is no cure for AMD, new treatments are available. The most effective treatment is Low Vision Rehabilitation. Training and special devices can promote independence and a return to favorite activities.
WHAT IS DRY MACULAR DEGENERATION?
This most common type of AMD is called dry macular degeneration. It affects 90% of the people who have the condition. In the dry form, there is a breakdown or thinning of the retinal pigment epithelial cells (RPE) in the macula. In the dry type of macular degeneration, the deterioration of the retina is associated with the formation of small yellow deposits, known as drusen, under the macula. This phenomenon leads to a thinning and drying out of the macula, causing it to lose its function. The amount of central vision loss is directly related to the location and amount of retinal thinning caused by the drusen.
WHAT IS WET MACULAR DEGENERATION?
Wet macular degeneration is the more severe type of AMD. In this form of macular degeneration, the fine blood vessels in the choroid (this is a part of the eye behind the retina) underlying the macula begin to proliferate. When those blood vessels proliferate, they leak, and cells in the macula are damaged and killed. The cause of this process, called choroidal neovascularization, is unknown.
The oxygen supply to the macula is disrupted and the body responds by growing new, abnormal blood vessels. These begin to grow through the breaks of the membrane behind the retina towards the macula, often raising the retina. Leakage into the retina from newly forming blood vessels causes the membrane that is underlying the retina to break.

To visualize this, imagine the roots of a tree growing and spreading until they actually uproot a sidewalk. Then imagine rainwater seeping up throughout the cracks. These abnormal blood vessels (the “roots”) tend to be very fragile. They often grow, leak or bleed, causing scarring of the macula. This damage to the macula results in rapid central vision loss. Once this vision is destroyed, it cannot be restored.
With the “wet” type, the patient may see a dark spot (or spots) in the center of their vision due to blood or fluid under the macula. Straight lines may look wavy because the macula is no longer smooth. Side or “peripheral” vision is rarely affected. Some patients, however, do not notice any such changes, despite the onset of neovascularization, Therefore periodic eye examinations are still very important for patients at high risk.
Although “wet” macular degeneration afflicts only 10 percent of those who have the condition, it accounts for 90 percent of the blindness caused by this disease.
DOES HEREDITY AFFECT MACULAR DEGENERATION?
As people age, their chances for developing various eye diseases increase dramatically. More recently, researchers have discovered that a significant number of these individuals may also have a major genetic component that contributes to the disease.
There are several hereditary forms of macular degeneration which, even though they are much less common, usually affect children or teenagers. Collectively, they are called Juvenile Macular Degeneration. Some of them are known as Stargardt’s Disease, Best’s Disease, and Sorsby’s Disease. Unfortunately, the specific factors that cause macular degeneration are not conclusively known and research into this little-understood disease is limited by insufficient funding.
WHAT THE PATIENT MAY SEE
NORMAL VISION

MACULAR DEGENERATION

Center vision may appear blurry because parts of the macula have begun to die, leaving blank spots in vision. Straight lines may look wavy. Side or “peripheral” vision is rarely affected.
WHAT IF I SHOW EARLY SIGNS OF MACULAR DEGENERATION?

The retina contains an extraordinary photosensitive array of cells that line the back of the eye. Light falling onto these cells in the retina is transformed into electrical signals which are transmitted to the brain centers that process and interpret them.
The most concentrated collection of photosensitive cells in the retina, including those that enable critical color and fine detail vision, are found in the Bulls-Eye center zone in an area called the macula.
WHAT ARE THE SYMPTOMS OF MACULAR DEGENERATION?
- A dark empty area in the center of vision
- Blurring and diminished colors in central vision
- Distortion of lines and shapes
- Difficulty in seeing detail up close and at a distance
In some cases, only one eye loses vision while the other eye continues to see well for many years. In its early stages the condition may be hardly noticeable, but when both eyes are affected, reading, close up work, driving and other normal daily activities can become difficult.
In most cases, patients report that their first sign of AMD was the rapid onset of prolonged, distorted vision. Straight lines like telephone wires and door frames appear to be wavy. A certain percentage of patients with wet AMD can benefit from laser treatment if the blood vessel leak is caught early enough. Both traditional photocoagulation laser and newer photodynamic therapy, using a photosensitive drug and a cold laser, can be effective in certain cases. There are even some new treatments under development for dry AMD.
In the human eye, light enters through the clear front surface of the eye (the cornea), passes through the opening of the pupil, through the lens and finally is perceived by the retina in the back of the eye. The retina is a multilayered structure that lines the inside of the globe. It is made up of specialized cells that convert the light to electrical impulses that travel to the brain and produce sight.
In the center of the retina, there is a tiny, extremely specialized area called the macula. It is approximately 1/8 inch in diameter. The macula has the most densely packed photoreceptors, cells that collect light. They consist of rods and cones, which also perceive color. The macula is supplied with oxygen-rich blood that nourishes the cells.
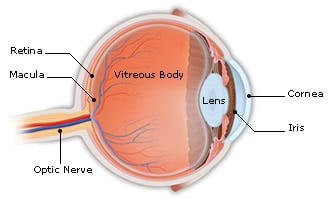
If the macula is intact, the eye sees the fine details of whatever is directly in front of it. Macular degeneration involves the deterioration or breakdown of this tiny structure. Central vision becomes blurred or disappears. Straight lines look wavy or broken. The edges of images are seen, but not what is in the middle. In time, the sense of color is diminished because the cones are damaged. The patient does not experience total blindness and there is always a ring of peripheral vision. However, vision may be reduced to legal blindness, which is vision of 20/200 or less with correction.
Because the brain cleverly learns to compensate and fill in the missing part of the picture in early cases with spotty macular cell damage or dysfunction, most people only visit their ophthalmologist when the disease is fairly advanced.
WHAT CAN YOU DO IF DIAGNOSED WITH MACULAR DEGENERATION?
- Detail a low-fat, low cholesterol diet.
- If you are post menopausal, consult with your physician concerning estrogen replacement therapy. This may have a favorable impact upon cholesterol lipid levels that play a role in worsening the disease.
- Wear sunglasses with UV protection.
- Try to consume at least two servings of leafy dark green vegetables per day.
- Do not smoke and avoid exposure to secondhand smoke. Smoking can reduce vital blood supply by contributing to narrowing of the blood vessels and thickening of the blood.
- Eat food and or supplements rich in vitamin E,C and Lutein. Lutein is a plant antioxidant found in high quantities in spinach, kale and other dark green, leafy vegetables
ARE THERE ANY SPECIAL RISK FACTORS FOR MACULAR DEGENERATION?
- History of hypertension
- History of cardiovascular disease
- Smoking
- Sun Exposure
- Lens Opacities (cataracts)
- Hyperopia (farsightedness)
- Light Skin & Eye Color
CAN MACULAR DEGENERATION BE PREVENTED?
At present, there is no known way to prevent macular degeneration. For now, the most important thing to do is to have regular eye exams, which may allow early detection and diagnosis. This is particularly important if a close relative has been diagnosed with macular degeneration.
There are also several areas of research that offer tremendous promise for halting the disease or restoring vision loss:
- Retinal Cell Transplants
- Pharmaceutical therapy
- Nutritional Therapy
- Gene Therapy